Rabies, a deadly viral disease, has been a persistent global health concern for thousands of years. While it is considered a neglected tropical disease, rabies can affect communities worldwide, particularly those lacking adequate surveillance, prevention, and control measures. Understanding the transmission of rabies is crucial in preventing future outbreaks and protecting ourselves from this deadly infection.
Rabies is an unpredictable disease with distinct stages of infection. It begins with an incubation period that can last from days to months, followed by flu-like symptoms. As the disease progresses, severe neurological effects set in, causing coma and ultimately leading to death. Early-stage symptoms are often nonspecific, such as fatigue, fever, and nausea. Neurological symptoms may include aggression, confusion, difficulty swallowing, and paralysis.
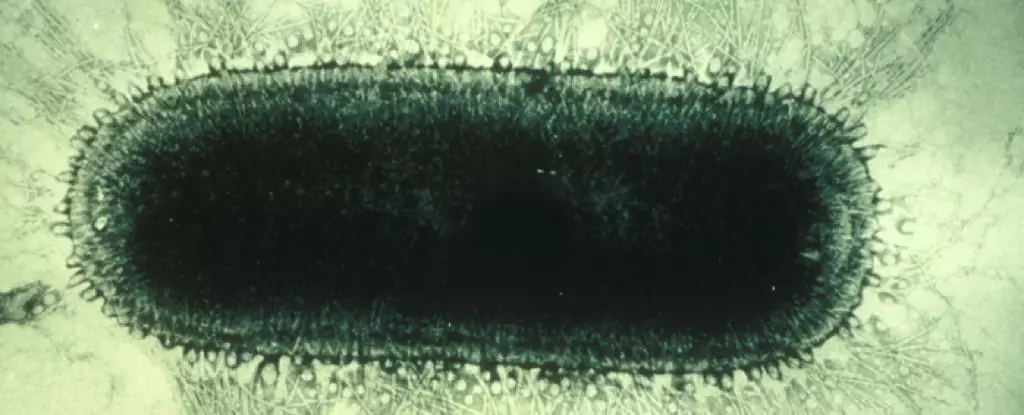
Rabies is caused by Lyssavirus, a genus of viruses that target warm-blooded vertebrates. While all mammals are susceptible to infection, only certain animals serve as reservoirs where the virus can multiply and transmit. In the United States, skunks, bats, foxes, coyotes, and raccoons are the highest-risk animal reservoirs for rabies.
The primary mode of transmission to humans is through animal bites. However, contact with open wounds or the mucous membranes of the eyes, nose, or mouth can also lead to infection. Once the virus enters the body, it replicates in muscle tissue and can make its way to the brain, causing severe inflammation and ultimately leading to death.
Measuring the global burden of rabies is challenging due to inadequate surveillance. However, while human rabies cases are rare in the United States, causing an average of one to three deaths per year, the disease claims tens of thousands of lives annually worldwide. In 2021, 54 U.S. jurisdictions reported 3,663 cases of rabid animals, showing an 18.2% decrease from the previous year.
Lower- and middle-income countries face additional challenges in controlling rabies, especially with disruptions to animal vaccination programs due to vaccine production and access issues. The COVID-19 pandemic has exacerbated these difficulties, leading to increased feral animal populations and a rise in human rabies cases in several countries.
Multiple ecological and socioeconomic factors contribute to the spread of rabies. Proximity to urban populations and transportation hubs has been associated with higher rabies cases in places like China. Climate change also plays a role by altering animal ranges, leading to increased interactions between susceptible animals and humans. As temperatures rise, tropical species like vampire bats expand their distribution, while Arctic species like red and Arctic foxes interact more frequently, potentially causing outbreaks.
Other factors such as increased human-animal interactions, lack of rabies education and prevention measures, and low levels of vaccination coverage further increase the risk of infection.
Historical attempts to control rabies through animal culling have proven ineffective and raised concerns regarding ethics, economics, and ecology. Animal vaccination, however, has shown promising results. Oral rabies vaccination of wildlife, initiated in the 1970s, successfully controlled rabies in coyote, fox, and raccoon populations in Europe and North America. Efforts have also been made to develop oral vaccines for dogs in countries like India and Thailand.
Prevention through education and vaccination is critical since no proven treatment for rabies exists. Preexposure prophylaxis (PrEP) involves exposing the immune system to a harmless version of the virus, offering protection against future infections. People working in high-risk occupations, such as wildlife biologists and veterinarians, are recommended to receive two doses of a rabies vaccine. Booster doses may be necessary for individuals at elevated risk of exposure.
Postexposure prophylaxis (PEP) involves administering a vaccine and medications after exposure to prevent infection. This includes a dose of human rabies immune globulin (HRIG) and multiple doses of the rabies vaccine. Regular pet and livestock vaccinations also play a crucial role in preventing rabies virus exposures.
There are several practical steps individuals can take to protect themselves from rabies:
1. Vaccinate and supervise your pets to prevent them from transmitting the disease.
2. Avoid handling wild animals that exhibit strange behavior as they may carry the virus.
3. Do not touch sick, injured, or dead animals.
4. Refrain from feeding wildlife, as this may encourage their presence.
5. Treat animals with respect by not teasing, disturbing their sleep, or handling their offspring.
6. Report any animal bites to an animal control officer, game warden, or healthcare professional.
Rabies remains a dangerous and deadly disease, but with the right knowledge and preventive measures, outbreaks can be controlled. Vaccination, both for animals and humans, is a crucial tool in preventing the spread of rabies. Education and awareness play a significant role in reducing the risk of infection. By implementing practical measures and fostering a global commitment to rabies control, we can work towards a safer future, free from the threat of rabies.
Leave a Reply