In a groundbreaking study, researchers in China have made significant strides in understanding how to restore brain function after cardiac arrest, demonstrating the remarkable potential of utilizing the liver in resuscitative processes. The research highlights that the activity in the brains of pigs was revived nearly an hour after cessation of blood flow, with some functionality sustained for hours. This finding not only extends the window of opportunity for effective brain resuscitation post-cardiac arrest but also opens new avenues for further exploration in neuroprotection and organ interdependence.
Sudden cardiac arrest is a critical medical emergency characterized by the abrupt loss of heart function, which leads to a swift cessation of blood circulation. This rapid decline in blood flow results in a phenomenon known as ischemia, particularly concerning when it affects the brain. Neurons, which are highly metabolically active cells, can sustain irreversible damage within mere minutes without adequate oxygen and nutrients. The conventional wisdom has emphasized the urgent need for immediate resuscitation due to this narrow therapeutic window, as prolonged ischemia can lead to devastating neurological deficits or death.
Traditionally, the focus has been on individual organs during recovery from ischemia, particularly the brain and heart. However, many studies suggest that the interplay between different organs could be critical in determining recovery outcomes. The latest research underscores the integral role of the liver in maintaining cerebral viability during resuscitation. While previous investigations have examined the effects of multi-organ ischemia, the specific roles of various organs, including the liver, had not been extensively evaluated. This study fills that gap and sheds light on the complicated dynamics that govern organ recovery after a cardiac event.
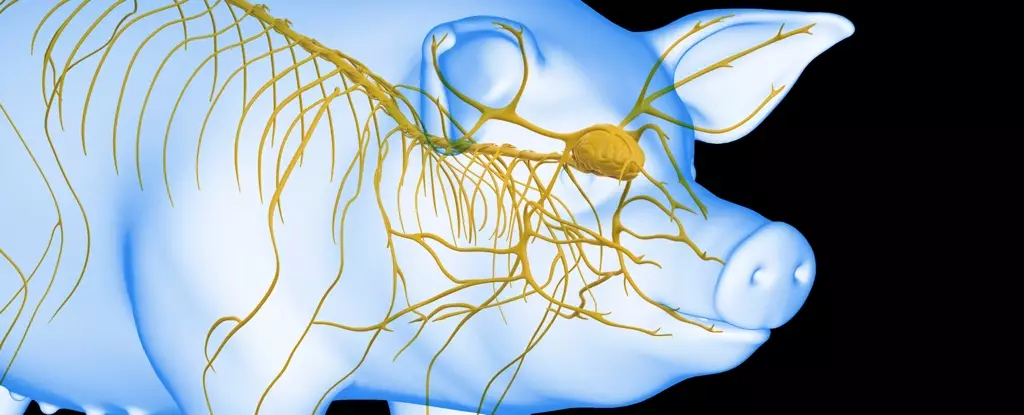
The pivotal study, which originated from Sun Yat-Sen University under the guidance of physician Xiaoshun He, utilized 17 lab-raised Tibetan minipigs to model human cardiac arrest scenarios. The researchers explored the effects of infusing liver function into the life-support regimen for the brain. They orchestrated a series of meticulously controlled experiments where two groups of pigs underwent brain ischemia, one also experiencing liver ischemia while the other did not. The evaluation proceeded to include a control group without any ischemic events, allowing researchers to delineate the effects of liver assistance on brain recovery.
Following euthanasia, the analysis of the brain tissue revealed that the pigs subjected to liver ischemia had significantly more considerable brain damage compared to those whose livers remained functional during the experiment. This pivotal finding suggested that the liver might play a critical protective role in mitigating brain injury during ischemic episodes.
The subsequent phase of the research entailed a more advanced life-support system that integrated an undamaged pig’s liver in reviving brains post-euthanasia. Utilizing an artificial heart and lung system allowed for the perfusion of fluids through the brain, simulating a biological environment optimized for recovery. This groundbreaking method, termed liver-assisted brain normothermic machine perfusion, involved testing various post-circulation delays. Specifically, the researchers sought to determine the maximum window in which brain electrical activity could be recovered when the liver was operational.
The most impressive result came from connecting the brains to the liver-integrated system 50 minutes post-circulation cessation—downstream from the critical 10-minute mark where initial brain activity started to decline. This interval heralded a remarkable re-emergence of brain activity that lasted six hours, with promising implications for future clinical scenarios.
The researchers concluded that the liver’s involvement has a paramount role in decreasing neurogenic injury following cardiac arrest. This pioneering discovery signifies a potential paradigm shift in the treatment of patients who have suffered from sudden cardiac arrest. By understanding and harnessing the organ interdependence, future research could lead to innovative therapies that extend the time frame for effective resuscitation and improve neurological outcomes.
Considering the profound implications of this study, further investigations are warranted to explore the underlying mechanisms at play and to establish protocols that can integrate this knowledge into clinical practice. The hope is that findings from such research will enhance survival rates and rehabilitative potential for human patients, paving the way for more resilient healthcare practices.
The fusion of organ science and neurology highlighted in this study paints an optimistic picture for the management of cardiac arrest, making this research a landmark in the field of emergency medicine.
Leave a Reply