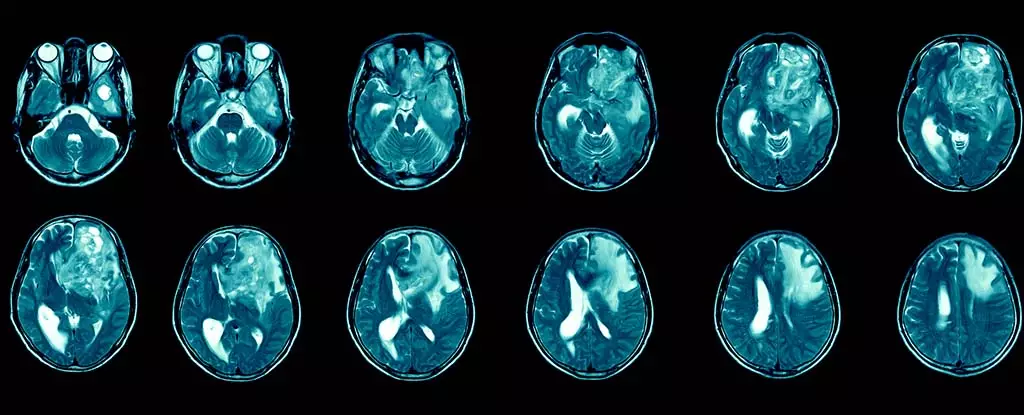
Glioblastoma multiforme (GBM) is recognized as one of the most aggressive and common types of brain cancer. It primarily affects adults and presents a stark reality for those diagnosed. Survival rates are painfully low; the prognosis indicates that the average patient lives only 12 to 15 months post-diagnosis. The most alarming statistic is that a mere 6.9% make it past the five-year mark. These figures highlight not just the immediacy of the medical challenge, but also the emotional and psychological toll on patients, caregivers, and families.
Beyond survival rates, the effects of glioblastoma can severely impair an individual’s quality of life. Symptoms often include debilitating headaches, seizures, cognitive decline, and significant changes in personality. These conditions can lead to a profound decrease in functional independence and overall well-being. Therefore, there’s an overwhelming demand for more effective treatment options as traditional methods fall short.
Current treatment strategies for glioblastoma typically involve a combination of surgical resection, radiation therapy, and chemotherapy. However, these treatments often yield only transient benefits. The inherent resilience of glioblastoma can be attributed to its ability to evade immune responses and the formidable blood-brain barrier, which limits the efficacy of systemic drugs.
Post-surgical recurrences of the tumor are common, leading to a never-ending cycle of treatment options that often provide little long-term relief to patients. This persistent battle underscores the urgent need for the development of targeted therapies that can effectively address this aggressive cancer.
Amidst the bleak landscape of glioblastoma treatment, immunotherapy is emerging as a beacon of hope. This innovative approach leverages the body’s immune system for the purpose of identifying and destroying cancer cells. Ongoing research is exploring ways to adapt immunotherapy for glioblastoma, signifying a pivotal shift in treatment paradigms.
Immunotherapy is not new; it has already been successfully implemented in the treatment of other cancers, including melanoma and lung cancer. The concept of applying similar strategies to glioblastoma presents both promise and complexity. One of the most challenging aspects of glioblastoma is its heterogeneous nature, with populations of cells that present different genetic mutations even within the same tumor. This diversity complicates the development of effective therapies, as a treatment that targets one mutation might overlook others.
Recent clinical trials have provided optimistic insights into the potential of immunotherapeutic delivery methods, such as injections into the cerebrospinal fluid. This approach aims to bypass the blood-brain barrier, attempting to provide localized treatment directly to the central nervous system.
Although the prospects of immunotherapy are thrilling, significant challenges remain. Research in brain cancer has been historically underfunded, limiting advancements. To combat this, interdisciplinary initiatives are being fostered to attract new researchers from various fields who can bring fresh perspectives to glioblastoma challenges.
One such researcher, who has spent two decades exploring the immune system’s intricacies during cancer and chronic infections, has shifted focus to glioblastoma. This shift represents a growing recognition that diverse academic and clinical expertise is essential to overcoming the hurdles posed by this formidable disease. By investigating how immune responses and brain functions interact, innovative strategies can be developed to effectively deliver immunotherapy and circumvent treatment barriers.
The need to approach glioblastoma treatment holistically is paramount. Understanding that treating brain cancer may not only require targeting tumor cells but also managing immune-related side effects is crucial. For example, methods such as injecting therapies into the bloodstream rather than direct brain surgery could be transformative, as it minimizes risks and enhances patient safety.
As researchers dive deeper into the potential of immunotherapy, the atmosphere characterizing glioblastoma treatment is gradually changing. With increased interest and investment in novel therapeutic approaches, the hope for better treatment outcomes continues to grow. However, it is essential to proceed with cautious optimism, considering both the complexities of the disease and the multifactorial nature of immune responses.
Ultimately, while glioblastoma remains a daunting challenge to treat, the ongoing commitment to harnessing innovative strategies through immunotherapy could pave the way for breakthroughs that improve the lives of countless patients suffering from this devastating disease. Collaborative research efforts and a multisectoral approach hold the key to unraveling the complexities and unlocking new avenues for effective treatments.

Leave a Reply