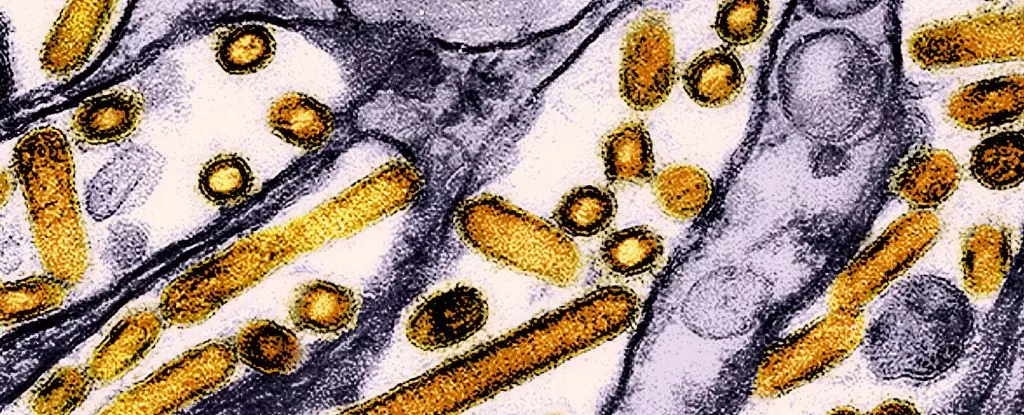
Recent investigations into the health of dairy workers in Michigan and Colorado have uncovered alarming evidence of human exposure to the highly pathogenic H5N1 avian influenza virus. According to research conducted by the US Centers for Disease Control and Prevention (CDC), blood samples from 115 individuals revealed that approximately 7 percent possessed antibodies indicating prior infection with this virulent strain of bird flu. This revelation not only highlights an emerging health risk but also calls into question the efficacy of current monitoring and preventive measures, exposing potential gaps in worker safety protocols.
The presence of antibodies does insinuate a level of exposure; however, it is worth noting that many of those affected did not report severe illness. In fact, about half of the individuals with detected antibodies indicated they experienced only mild symptoms, suggesting that while the spread of H5N1 may have gone unnoticed, its immediate health implications for most remain low. Still, this should not provide a false sense of security; the nonchalance towards mild infections could breed complacency regarding the virus’s potential to evolve into more dangerous variants.
Increasingly concerning are reports from Cambodia, where a deadly hybrid strain of bird flu—combining two virulent lineages—has resulted in multiple fatalities. This development underscores the mutable nature of viruses, particularly when given opportunities to evolve amidst populations with insufficient controls. The hybrid strain, shown to possess mutations enhancing its capacity for airborne transmission, signals a need for vigilance. Outbreaks like these serve as critical reminders that seemingly isolated incidents can be harbingers of broader health crises, especially when related to zoonotic diseases.
Despite the ongoing outbreak in Cambodia, with no evidence so far of human-to-human transmission, the potential for changes in virulence and transmission dynamics remains a genuine concern. Meanwhile, the Canadian case of a teenager hospitalized with a mutated variant of H5N1 adds another layer of urgency to the situation. Genetic sequencings revealing changes that enhance the virus’s ability to infect humans necessitate comprehensive monitoring and rapid response strategies to mitigate further spread.
The factors contributing to the silent spread of the avian influenza among dairy workers cannot be ignored. Most notably, a glaring lack of adherence to recommended personal protective equipment (PPE) has been observed among these individuals. Despite clear guidelines from health authorities, reports indicate that none of the infected dairy workers consistently utilized PPE while working in proximity to infected animals. This neglect presents an alarming risk to both workers and their communities, as it not only jeopardizes their health but also facilitates the possibility of the virus flourishing unchecked.
Moreover, the alarming gallop of H5N1 across 48 US states, infecting over 400 dairy herds, highlights a systemic issue within agricultural practices where health guidelines may not be adequately enforced or respected. Therefore, proactive outreach and educational initiatives need to be culturally tailored, particularly aimed at Spanish-speaking workers who constitute a significant portion of this workforce. Simple yet effective outreach could ensure that this vulnerable group is well-informed about the risks and the requisite safety measures.
In light of these findings, authorities are urged to act decisively. The global community must prioritize animal health surveillance as well as robust worker education regarding biosecurity practices. Enhanced monitoring systems should be established to ensure rapid identification of outbreaks, accompanied by resources geared towards improving safety compliance in agricultural settings.
Furthermore, the need for a human vaccine emerges as a critical component of comprehensive pandemic preparedness. With the avian influenza exhibiting traits that may promote virulence and human infection, the development of preventive measures must include not just the vaccination of at-risk animals but also effective vaccines for humans. In doing so, authorities can mitigate the health risks posed by this emerging threat.
Finally, it is imperative for individuals to exercise good hygiene when engaging with animals and to report any unusual occurrences of sick or dead birds to the relevant authorities. The observance of the signs of infection—including lethargy and coordination issues in animals—could ultimately play a crucial role in curbing the spread of avian influenza.
The situation surrounding the H5N1 outbreak serves as both a wake-up call and a clarion call for more stringent health policies and community education. The intersection of human and animal health must be approached with an integrative mindset, as we navigate the complex landscape of infectious diseases in an increasingly interconnected world.

Leave a Reply