In recent years, the use of selective serotonin reuptake inhibitors (SSRIs) as a primary treatment for mood disorders such as depression and anxiety has become increasingly prevalent. Millions of individuals rely on these medications to improve their mental health. However, the controversy surrounding SSRIs stems from a lack of comprehensive data regarding their long-term efficacy, the clear understanding of their mechanisms of action, and the actual mood enhancement they may provide. A recent study conducted by Vibeke Dam and her colleagues at Copenhagen University aims to shed light on these issues by investigating the cognitive effects associated with SSRI use, particularly focusing on a commonly prescribed medication, escitalopram.
The study observed 90 patients suffering from moderate to severe depression. They underwent extensive evaluations, including cognitive and mood assessments, along with brain scans prior to initiating treatment with escitalopram. This initial assessment serves as a baseline to identify changes attributable to the medication after an eight-week period. At the conclusion of this treatment phase, researchers repeated the cognitive and brain assessments for a subset of 40 participants.
Surprisingly, results indicated a nearly 10 percent reduction in the binding of serotonin receptors in the brain, particularly the 5HT4 receptor, after treatment. Most notable was the improvement in verbal memory amongst those who demonstrated minimal change in receptor levels. This hints at a nuanced relationship where receptor availability does not directly correlate with mood improvement but may play a significant role in cognitive function.
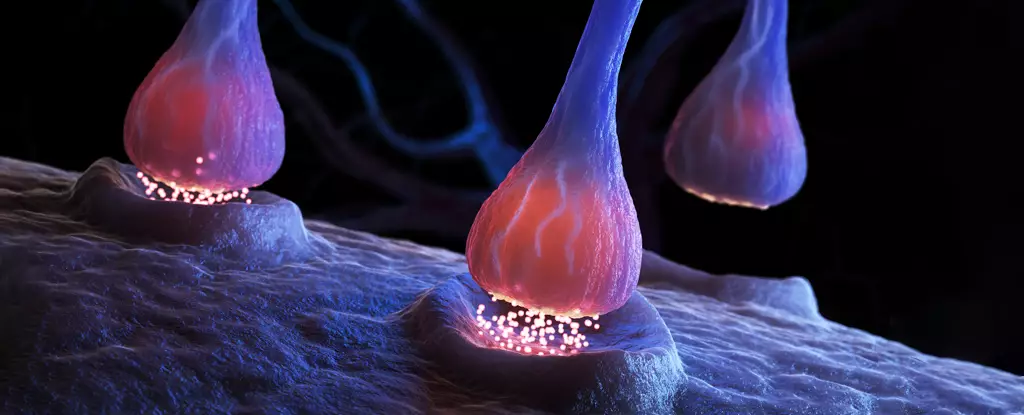
The researchers were keen to highlight that the enhancement in cognitive function could potentially be directly related to the dynamics of the 5HT4 receptor. Vibeke Dam stated, “Our work ties the improvement in cognitive function to the specific 5HT4 receptor.” By increasing serotonin levels in synapses, SSRIs may enhance the efficiency of remaining serotonin receptors, including 5-HT4, thereby improving cognitive abilities without necessarily alleviating depressive symptoms.
What stands out in the findings is the disconnect; while cognitive functions such as word recall showed measurable improvement, mood or emotional state did not reflect a parallel enhancement. This divergence raises critical questions about the true efficacy of SSRIs in treating the overall spectrum of depression. Could it be that patients are experiencing a cognitive boost without an equivalent emotional uplift?
Despite the promising insights from this study, it is vital to acknowledge the ethical considerations that limited the research scope. The absence of a placebo group challenges the certainty of attributing the benefits solely to escitalopram. Identifying whether the cognitive improvements were genuinely due to SSRIs or if they were influenced by other variables remains uncertain.
Furthermore, previous research has pointed out troubling evidence questioning the efficacy of SSRIs. Some studies suggest that these medications do not substantially outperform placebo treatments, igniting a larger debate over the fundamental role of serotonin in mood disorders. This controversy calls for a more nuanced investigation into how antidepressants function and whether SSRIs are even a cornerstone of effective treatment.
It is essential to tread cautiously regarding treatment adjustments. Patients relying on SSRIs should always seek professional advice before making changes to their medication regimen to avoid any serious health repercussions. Given the complexities outlined, further research is crucial in elucidating the mechanisms through which SSRIs operate. The study’s authors emphasize the necessity for ongoing investigation to uncover the precise actions of both SSRIs and alternative treatment strategies.
As we delve deeper into the world of antidepressants, it becomes increasingly clear that understanding their effects—especially regarding cognitive processes and mood stabilization—is vital in advancing public health strategies. There remains a pressing need for research that not only scrutinizes current treatments but also explores innovative interventions tailored to individual needs in the ever-evolving landscape of mental healthcare. The findings from this study, while preliminary, serve as a stepping stone towards optimizing how we approach the treatment of mood disorders, with the hope of achieving truly effective outcomes for patients.

Leave a Reply