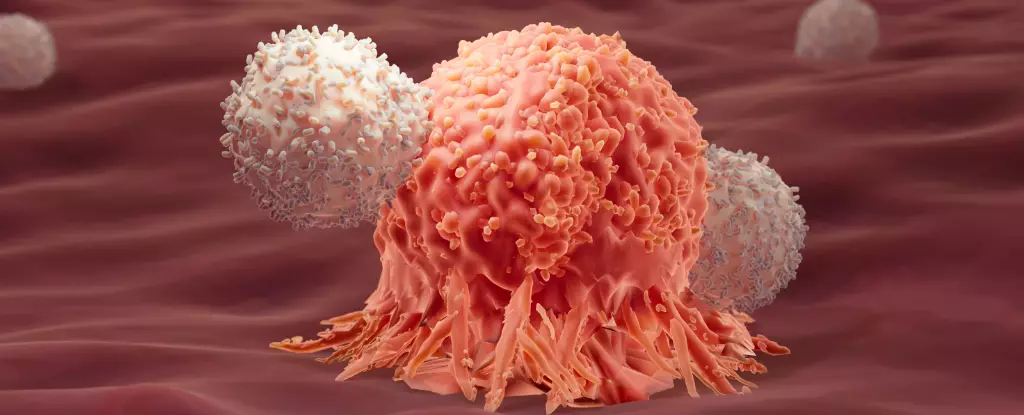
Recent advancements in the realm of cancer treatment have unveiled a compelling narrative surrounding the immune system’s functionality, particularly emphasizing the intriguing interplay between differing immune responses. Two pivotal studies have emerged, suggesting that a deeper understanding of these immune interactions may significantly enhance cancer patients’ survival prospects, tapping into a unique immune phenomenon often dismissed as counterproductive. This article explores the insights gleaned from these studies and their implications for future cancer therapies.
Immunotherapy represents one of the most promising frontiers in cancer treatment, leveraging the body’s innate defenses to combat malignancies. Specifically, techniques such as CAR-T cell therapy have revolutionized how oncologists approach cancers, particularly leukemias. The foundational principle behind CAR-T therapy involves harvesting T cells from a patient’s blood, modifying them to recognize and target cancer cells more effectively, and subsequently reinfusing them into the patient. However, the effectiveness of this therapy can vary widely, with nearly half of patients suffering from acute lymphoblastic leukemia (ALL) experiencing a relapse within a year post-treatment. This unpredictability has led researchers to investigate the characteristics of patients who experience sustained remissions, ultimately revealing a fascinating connection to a rarely acknowledged aspect of immune response.
Traditionally, the immune system’s response to cancer is predominantly categorized into two types: Type 1 and Type 2. Type 1 responses are generally recognized as the frontline defense against cancerous cells, targeting intracellular threats with remarkable precision. Conversely, Type 2 responses are often associated with combating larger parasitic organisms and have historically been seen as irrelevant or detrimental to cancer management. However, the recent studies conducted by researchers at the École Polytechnique Fédérale de Lausanne (EPFL) revealed that long-term remission in certain patients coincided with the presence of Type 2 immune markers.
The surprise finding suggests that these Type 2 immune factors, typically deemed ineffective against cancer, may in fact play a crucial role in promoting prolonged remission. The correlation does not imply causation but posits a synergistic relationship between Type 1 and Type 2 immune responses, akin to the philosophical concept of yin and yang. This concept emphasizes balance and harmony, shedding light on the complex dynamics of our immune system in fighting cancer.
In a rigorous follow-up study, researchers applied this dual response concept to experiments involving mice suffering from colon adenocarcinoma, a form of solid tumor notorious for its resistance to conventional immunotherapy. The results were astonishing: a combination therapy utilizing both Type 1 and Type 2 immune responses resulted in an 86% cure rate among the treated mice. In contrast, those subjected solely to Type 1 responses demonstrated a dismal survival rate, with none enduring beyond a few weeks.
A noteworthy aspect of this combinatorial approach was the enhancement of a metabolic pathway called glycolysis, which appears to furnish T cells with enhanced energy levels. This energy boost might enable the immune cells to maintain their combat efficiency against cancer while alleviating the exhaustion that often accompanies prolonged immunotherapy.
The implications of these findings extend far beyond laboratory results. Should the synergistic interaction between Type 1 and Type 2 immune responses prove replicable in human trials, this could herald a transformative shift in how oncologists design immunotherapies. The potential to incorporate Type 2 immune elements into cancer treatment regimens may offer hope to those patients who have experienced inadequate responses to traditional methods.
While these studies represent exciting progress, researchers caution against drawing premature conclusions. The identification of a correlation does not equate to a definitive pathway for treatment design. Further investigations are necessary to elucidate the underlying mechanisms and translate these findings into viable clinical practices.
The evolving landscape of cancer immunotherapy encapsulates a dynamic interplay between various immune responses. By redefining our understanding of Type 1 and Type 2 immunity, researchers are paving the way for innovative treatment modalities that could enhance survival rates for cancer patients. Embracing the complexity of the immune system, as illustrated by the yin and yang metaphor, invites a more holistic approach to combating one of humanity’s most formidable health challenges.

Leave a Reply