Long COVID is a complex and debilitating illness that continues to puzzle researchers and healthcare professionals around the world. Contrary to initial beliefs that it may be psychosomatic, recent studies are shedding new light on the biological mechanisms underlying this condition. In a groundbreaking study conducted by researchers at the University of California, San Francisco, CellSight Technologies, and Kaiser Permanente South San Francisco Medical Center, the findings suggest that long COVID is not simply a figment of the imagination, but rather a real and tangible biological phenomenon.
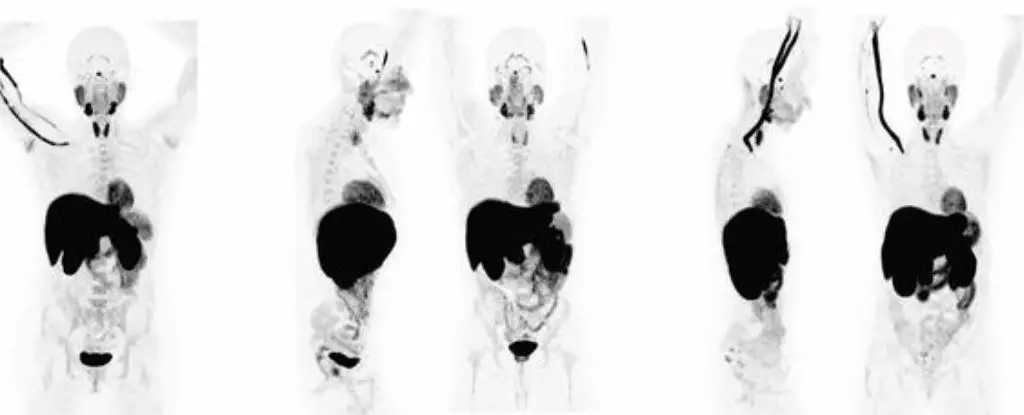
The study involved 24 patients who had recovered from COVID-19, and the results were eye-opening. A PET imaging test revealed abnormal T cell activity in various parts of their bodies, including the brain stem, spinal cord, bone marrow, nose, throat, lymph nodes, heart, lungs, and gut. Interestingly, these abnormal immune responses were present in both the participants experiencing long COVID symptoms and those who had fully recovered from the acute phase of the virus. The activation of immune T cells in certain tissues was significantly higher in patients with lingering symptoms, suggesting a direct correlation between immune activation and the persistence of long COVID.
One of the most concerning aspects of long COVID is the persistence of these abnormal immune responses. Even in patients who had fully recovered from the initial infection, changes in T cell activity were still evident in various organs, up to two and a half years post-infection. This highlights the long-term consequences that even a mild COVID-19 infection can have on the immune system and overall health. Researchers warn that this ongoing immune activity could potentially lead to the presence of an active viral reservoir in deeper tissues, further complicating the condition.
Challenges in Diagnosis
Diagnosing long COVID presents a significant challenge due to the multitude of symptoms that can manifest in patients. With over 200 reported symptoms ranging from ‘brain fog’ to persistent fatigue, memory loss, and gastrointestinal issues, distinguishing long COVID from other illnesses is no easy task. The overlap of symptoms with conditions like chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME) further complicates the diagnostic process. Additionally, autopsies of COVID patients have revealed the presence of the SARS-CoV-2 virus in various tissues throughout the body, underscoring the complexity of the disease.
Neurological Implications
Recent discoveries have linked long COVID to neurological abnormalities, with brain scans showing changes that mirror those seen in CFS/ME. The presence of T cell abnormalities in the spinal cord and brain stem suggests a direct involvement of the central nervous system in the immune response. This challenges the traditional view of COVID-19 as a transient infection and underscores the need for further research to confirm these findings in larger cohorts. The implications of these discoveries on the long-term health of COVID-19 survivors are profound and warrant continued exploration.
The biological toll of long COVID is a complex and multifaceted issue that requires a deeper understanding of the immune responses and viral persistence involved. By uncovering the underlying mechanisms of this condition, researchers can pave the way for more targeted treatments and interventions to alleviate the suffering of long COVID patients. As our knowledge of this disease continues to evolve, so too must our approach to managing and treating the long-term effects of COVID-19.

Leave a Reply