Alzheimer’s disease, a debilitating neurodegenerative disorder, has been the focus of extensive research in recent years. While much attention has been given to the immune system’s role within the brain, little has been explored regarding potential differences in white blood cells throughout the rest of the body. However, a recent study conducted by researchers from Northwestern University in the US has shed light on this matter. Their findings suggest that immune cells in the blood of individuals with Alzheimer’s disease display subtle changes in how their genes are read, possibly indicating the body’s preparation to combat the disease.
The Unraveling of DNA
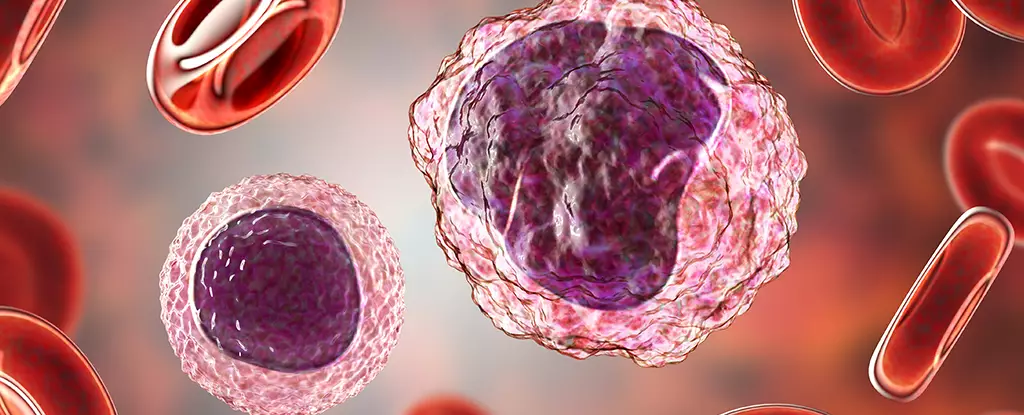
The Northwestern University researchers utilized single-cell gene translation technology to examine white blood cells taken from both healthy individuals and those diagnosed with Alzheimer’s disease. The study revealed that every type of white cell investigated in Alzheimer’s patients harbored epigenetic changes. Epigenetic changes refer to modifications in DNA chemistry that can either enhance or interfere with gene expression. In this case, these changes caused specific sequences within the cell’s chromosomes to be more easily read. Interestingly, these changes allowed certain genes to be exposed, potentially enabling the cells to interact with Alzheimer’s pathology.
The study identified a variety of genetic changes in different white blood cell types of Alzheimer’s patients. Monocytes, a type of large white cell, exhibited changes dependent on the apolipoprotein E genotype possessed by the individual. This genotype combination has been linked to an increased risk of developing Alzheimer’s disease. Additionally, CD8 T cells, another type of white blood cell, displayed distinct changes in those with the condition. Through specific epigenetic modifications, a membrane protein called CXC motif chemokine receptor 3 (CXCR3) stood out more prominently in Alzheimer’s patients. This protein guides the T cells towards the brain. Although the reasons behind the altered functioning of T cells are unclear, this observation provides potential clues as to why immune cells are typically restricted from entering the brain.
While T cells in the brain can be harmful, the researchers speculate that these cells may also be attempting to repair the brain damage. The presence of CXCR3 allows the T cells to home in on signals emitted by the damaged brain. However, the exact mechanisms and reasons for this behavior remain subjects of future research. Nonetheless, the discovery of these epigenetic changes opens new avenues for investigating the progression of Alzheimer’s disease and identifying potential therapeutic targets.
Implications and Future Research
The study’s findings suggest that the peripheral immune response may play a role in Alzheimer’s disease risk. Understanding the origins and impact of epigenetic changes in immune cells could offer valuable insights into the development and progression of the disease. Further research is needed to unravel the mechanisms underlying these genetic alterations and to determine whether they are indicative of brain pathology or precursors to the disease. Identifying therapeutic targets based on these findings could lead to the development of novel interventions to mitigate the effects of Alzheimer’s disease.
The intricate relationship between the immune response and Alzheimer’s disease is gradually unfolding. The Northwestern University study highlights the presence of epigenetic changes in white blood cells of Alzheimer’s patients, suggesting a potential link between peripheral immune cells and the development of the disease. The altered gene expression observed in different types of immune cells provides valuable insights into the mechanisms and potential targets for therapeutic intervention. Further exploration of these genetic changes will undoubtedly contribute to our understanding of Alzheimer’s disease and pave the way for innovative treatment strategies.

Leave a Reply