The menstrual cycle is a well-known biological process accompanied by a complex interplay of hormones that oversee various physiological changes. However, recent studies have unveiled a surprising connection between these hormonal fluctuations and structural transformations in the brain. Led by neuroscientists Elizabeth Rizor and Viktoriya Babenko from the University of California, Santa Barbara, a team has embarked on a pioneering study exploring how the menstrual cycle reshapes neural structures. While reproductive health remains crucial, understanding the broader impacts of these biological changes on mental health is essential, given that those who menstruate will experience an estimated 450 cycles in their lives.
Despite the prevalence of menstruation, scientific inquiry into its comprehensive effects on the brain has been notably scarce. Much of the existing research has focused primarily on cognitive functions and the brain’s communicative abilities during tasks, while neglecting the actual structural changes that occur within the brain itself. As Rizor, Babenko, and their associates emphasize, “Cyclic fluctuations in HPG-axis hormones exert powerful behavioral, structural, and functional effects through actions on the mammalian central nervous system.” This statement highlights a pressing need to delve deeper into the neurological implications of the menstrual cycle.
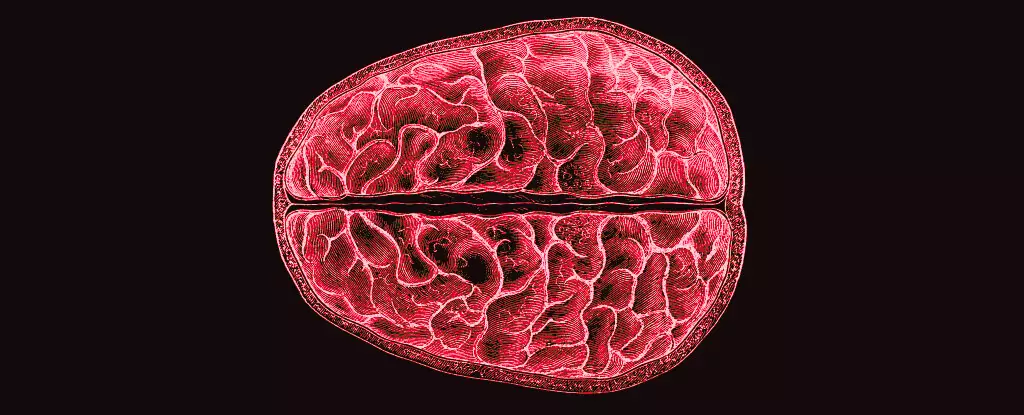
The study undertaken by Rizor’s team examined 30 menstruating individuals in order to assess brain changes across three distinct phases of the menstrual cycle: menses, ovulation, and mid-luteal. Utilizing advanced MRI technology, the researchers provided insight into how white matter microstructure—the network of neuronal fibers responsible for information transfer between different gray matter regions—varies with hormonal activity. This research is notable not just for its findings, but for its attempt to fill a significant gap in our understanding of menstrual cycles and their impact on the brain.
The study revealed that as hormone levels shifted, notable changes also occurred in both gray and white matter volumes, as well as the volume of cerebrospinal fluid. In particular, the days leading up to ovulation, characterized by elevated levels of hormones like 17β-estradiol and luteinizing hormone, were associated with structural modifications in the brain indicative of enhanced speed in information transfer across neural pathways. Meanwhile, the onset of follicle-stimulating hormone—which rises prior to ovulation—was linked with increased thickness in gray matter, suggesting a potential enhancement in cognitive processing capabilities during this phase.
While the implications of these structural modifications remain to be fully understood, the correlation between hormonal fluctuations and changes in brain architecture suggests a profound relationship that could affect behavior and mental health. Significantly, the hormonal rise after ovulation leads to increased progesterone levels, which in turn corresponded with an increase in brain tissue and a decrease in cerebrospinal fluid volume. Such alterations may influence mental states, particularly as they relate to mood and cognitive function.
The data gleaned from this research opens the door for more extensive studies that could explore, for instance, the underlying causes of extraordinary yet debilitating mental health conditions related to menstruation, such as premenstrual dysphoric disorder (PMDD). This severe condition, characterized by significant mood disturbances, often places those affected in challenging emotional and psychological states, suggesting a critical need for greater awareness of the menstrual cycle’s role in mental health.
As researchers continue to explore the fascinating connections between hormones and brain structure, an emphasis on holistic approaches is essential. Future studies should not only aim to uncover the acute impacts associated with hormonal changes but also promote a more nuanced understanding of the long-term consequences these transformations could have over an individual’s lifetime. The intricate interplay of hormone cycles and brain function necessitates research that crosses disciplinary boundaries, integrating insights from neuroscience, psychology, and gynecology.
The study spearheaded by Rizor and Babenko sets a powerful precedent for future exploration into the interplay between the menstrual cycle and the brain. Understanding hormone-driven brain changes represents an essential frontier in both neuroscience and women’s health, promising not only to amplify knowledge in these fields but also to enhance support for those navigating the complexities of menstrual health. It is vital that the scientific community continues to investigate this relationship, paving the way toward improved mental health strategies for those affected.

Leave a Reply