The association between cancer risk and lifestyle factors like diet and metabolic conditions has long been acknowledged. Recent research by scientists from Singapore and the UK sheds light on a previously unknown mechanism that explains why an unhealthy diet or unmanaged metabolic conditions, such as diabetes, can increase the risk of cancer. The study revealed that changes in glucose metabolism could play a crucial role in promoting tumor growth by temporarily disabling a gene called BRCA2, which is known to protect against tumors.
The findings of the study also challenge a well-established theory in the field of cancer genetics, known as Knudson’s ‘two-hit’ paradigm. According to this theory, both copies of a tumor suppressor gene must be permanently inactivated for cancer to develop. However, recent studies have shown that mutations in just one copy of the BRCA2 gene can increase the risk of various cancers. This raises questions about the traditional understanding of genetic factors that protect against cancer and highlights the need for further research in this area.
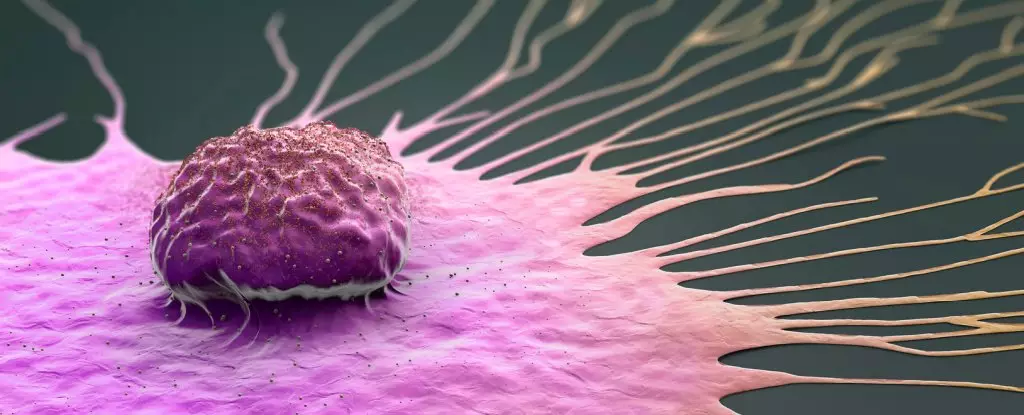
One of the key discoveries of the study was the role of methylglyoxal (MGO) in temporarily disabling the tumor-suppressing functions of the BRCA2 protein. MGO is a byproduct of glucose metabolism and is produced when cells break down glucose for energy. High levels of MGO can lead to the formation of harmful compounds that damage DNA and proteins, contributing to the development and progression of cancer. This effect was observed in noncancerous cells, patient-derived tissue samples, and animal models of cancer.
The findings of this study have important implications for cancer prevention and treatment. By understanding the role of glucose metabolism and MGO in inactivating tumor-suppressing genes, such as BRCA2, researchers may be able to develop strategies for early detection and prevention of cancer. The discovery that MGO can be detected through a simple blood test for HbA1C opens up possibilities for using this marker to assess cancer risk in individuals with two functional copies of the BRCA2 gene.
While the results of this study are promising, more research is needed to validate the findings on a larger scale. The researchers emphasize the importance of conducting further studies using clinical data and animal models to explore the links between dietary factors, metabolic disorders, and cancer risk. Understanding how environmental factors, such as high MGO levels due to diabetes, can increase the risk of cancer is critical for developing targeted interventions and improving patient outcomes.
The link between glucose metabolism and cancer risk represents a novel area of research with significant implications for cancer prevention and treatment. By unraveling the mechanisms through which MGO and other metabolic byproducts affect tumor-suppressing genes like BRCA2, scientists are paving the way for innovative approaches to cancer management. This study highlights the complex interplay between genetic factors, lifestyle choices, and metabolic conditions in shaping an individual’s risk of developing cancer.

Leave a Reply